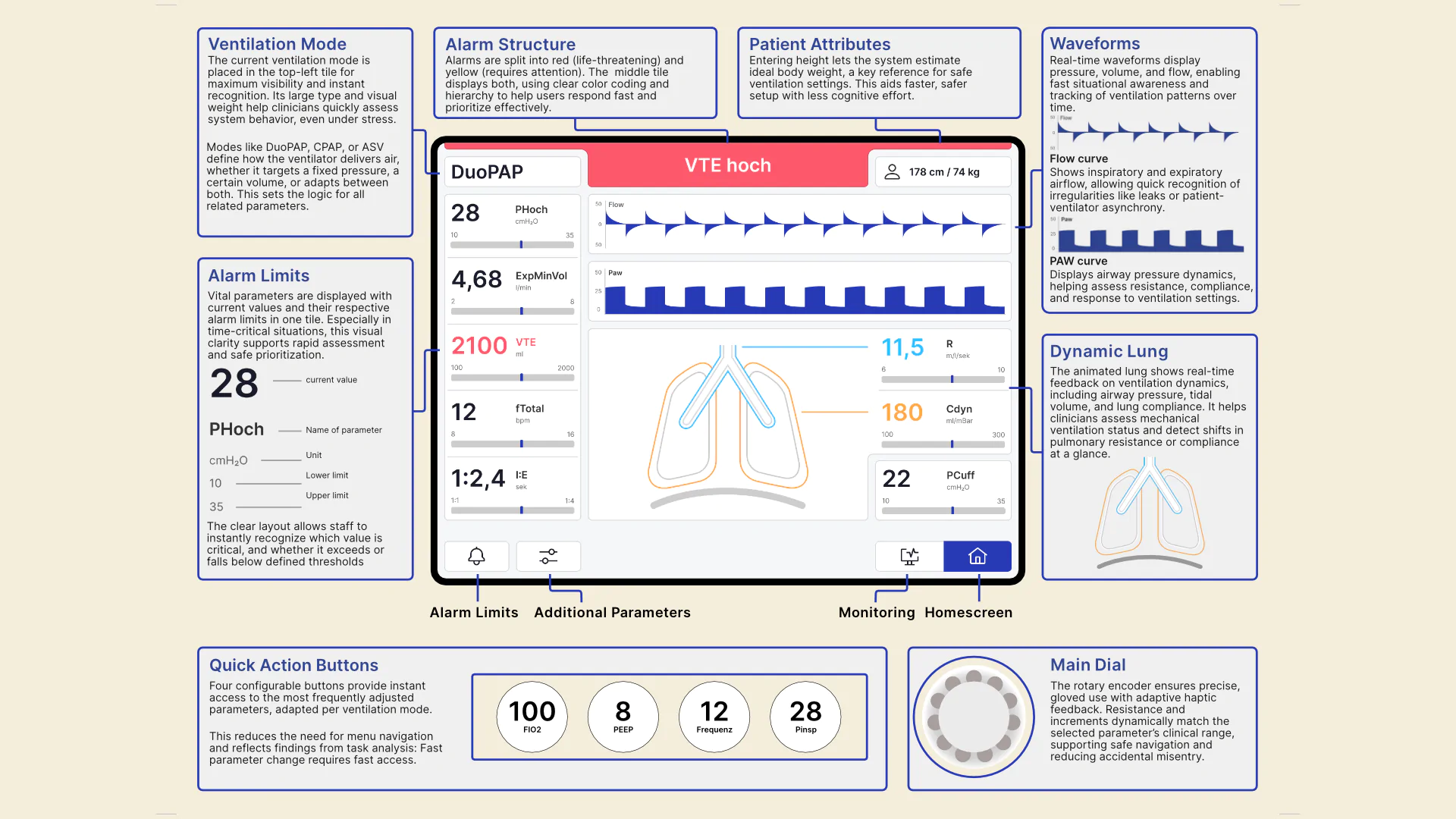
How do clinical staff orient themselves in critical situations, and what interface factors help or hinder rapid information uptake?

CuraVent
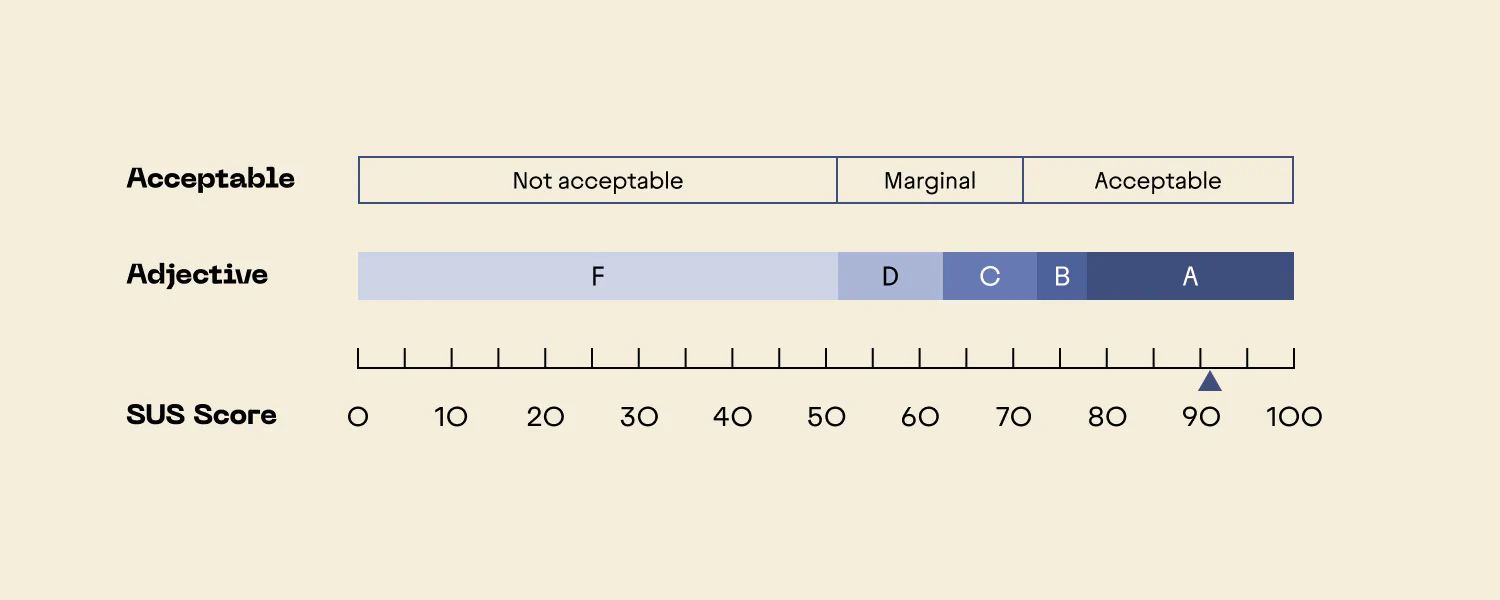
CuraVent is an evolutionary redesign of an ICU ventilator interface, designed to reduce cognitive load and support safe, rapid decision-making in critical care. Based on in-depth contextual research and task analysis, the interface was rebuilt around flat hierarchies, visual clarity, and tactile feedback. I led user research, clinical grounding, and usability evaluation. A hi-fi prototype was formative tested with ICU nurses and anaesthesiologists. Results showed a 40% faster setup time and a SUS score of 92, demonstrating that context-aware design interventions can meaningfully improve interaction quality in high-stakes environments.